“Learn how to navigate 2025 MIPS reporting, avoid costly Medicare penalties, and maximize incentives. Expert tips for healthcare providers from Medversify.”
2025 MIPS REPORTING
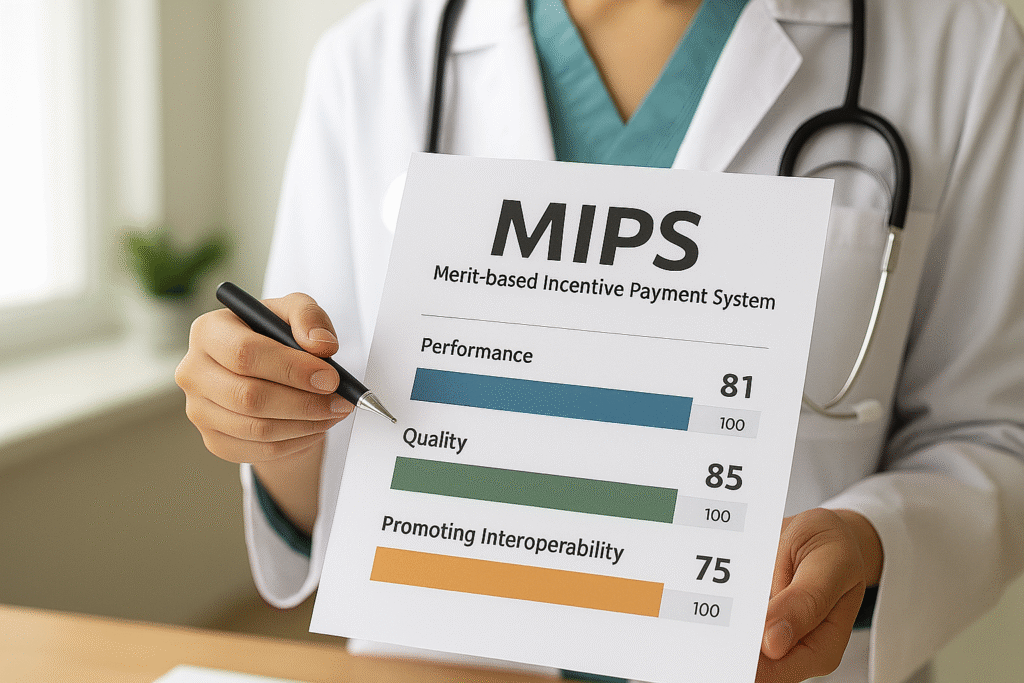
In 2025, the Merit-Based Incentive Payment System (MIPS) remains a key factor in your Medicare reimbursements. A high score can increase your revenue, while missing the mark can cost thousands in penalties. At Medversify, we help healthcare providers simplify MIPS reporting so they can focus on patient care — and keep their Medicare payments growing.
What’s New in 2025 MIPS Reporting?
CMS has made important updates you need to know:
- Performance Threshold: Still 75 points to avoid penalties.
- Data Completeness: 75% reporting rate remains until 2028.
- Quality Measures: 7 new measures added, 10 removed, 66 updated (total: 195 measures).
Common Mistakes That Lead to Penalties
- Missing Deadlines – Late submissions result in automatic penalties.
- Choosing the Wrong Measures – Selecting measures that don’t fit your specialty lowers your score.
- Low Data Completeness – Reporting less than 75% of eligible cases impacts points.
- Not Reviewing Feedback Reports – Overlooking CMS feedback can cause repeat mistakes.
Steps to Boost Your MIPS Score in 2025
- Start Early – Identify your measures and reporting method now.
- Use the Right Measures – Pick those aligned with your practice specialty.
- Track Performance Quarterly – Don’t wait until year-end to check progress.
- Leverage Expert Help – Partnering with MIPS consultants like Medversify ensures compliance and optimization.
Why Work with Medversify
We handle the complex reporting process from start to finish. Our clients:
- Avoid Medicare penalties.
- Increase their MIPS score for higher reimbursements.
- Spend more time on patient care, less on paperwork.
Conclusion
MIPS reporting doesn’t have to be stressful. With the right strategy, 2025 can be your most profitable year yet. Contact Medversify to get started with expert MIPS support today.
Free MIPS Performance Check: Ensure Your Practice is Positioned to Maximize Incentives and Avoid 2025 Medicare Penalties